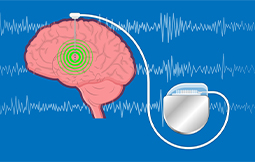
Deep brain stimulation includes implanting electrodes within certain areas of your brain. These electrodes produce electrical impulses that regulate abnormal impulses.
Deep brain stimulation includes implanting electrodes within certain areas of your brain. These electrodes produce electrical impulses that regulate abnormal impulses. Or the electrical impulses can affect some cells and chemicals within the brain. The amount of stimulation in deep brain stimulation is managed by a pacemaker-like device placed under the skin in your upper chest. A wire that travels under your skin attaches this device to the electrodes in your brain.
Deep brain stimulation is an established procedure for people with movement disorders, such as essential tremor, Parkinson’s disease and dystonia, and psychiatric conditions, such as obsessive-compulsive disorder. It’s also approved for use by the Food and Drug Administration to decrease seizures in difficult-to-treat epilepsy. This treatment is reserved for people who aren’t ready to get control of their symptoms with medications.
Before surgery, you’ll need medical tests to make sure that deep brain stimulation is a safe and appropriate option for you. You’ll also require brain-imaging studies, such as an MRI, before the surgery, to map the areas of your brain to implant the electrodes.
In usual, here’s how surgery for deep brain stimulation works:
Brain surgery: For the brain surgery portion, your care team fits you with a special head frame to hold your head still during the procedure (stereotactic head frame). Then, team members use magnetic resonance imaging (MRI) to map your brain and classify the area in your brain where they’ll place the electrodes. Surgery can be done under general anesthesia so that you’ll be unconscious. Or the procedure can be done with you awake and alert. If you’re awake for surgery, you’ll be given a local anesthetic to numb your scalp before the procedure, but you won’t need an anesthetic in your brain itself because the brain has no pain receptors.
Chest wall surgery: During the second portion of the surgery, the surgeon implants the portion of the device that contains the batteries (pulse generator) under the skin in your chest, near your collarbone. General anesthesia is used during this method. Wires from the brain electrodes are placed under your skin and led down to the battery-operated pulse generator.
A few weeks after surgery, the pulse generator in your chest is activated in your doctor’s office. The doctor can easily program your pulse generator from outside your body using a unique remote control. The amount of stimulation is customized to your condition and may take as long as four to six months to find the optimal setting. The stimulation may be constant, 24 hours a day, or your doctor may advise you to turn your pulse generator off at night and back on in the morning, depending on your condition.
Surgery risks
Possible side effects of stimulation
Copyright © 2021 IMA | All Rights Reserved.